Introduction to the Congo Illness
The Democratic Republic of the Congo (DRC) has recently grappled with a series of outbreaks of a mysterious illness, now commonly referred to as the Congo illness. Initially reported in various communities, this illness has manifested with alarming symptoms, raising concerns among healthcare professionals and local populations alike. The outbreaks have not only had dire health implications but have also instigated significant socio-economic challenges within the affected regions.
The Congo illness is characterized by a range of symptoms, including fever, fatigue, severe headaches, and respiratory issues, although the exact clinical picture can vary widely. In severe cases, patients have reported gastrointestinal complications and neurological symptoms. It is this variability that has made diagnosis challenging, contributing to the difficulty in addressing the outbreaks effectively. Due to the severity of symptoms, there have been a troubling number of associated fatalities, which has also compounded public anxiety surrounding the disease.
This introduction sets the stage for a deeper exploration of the Congo illness, its origins, and the potential causes fueling its re-emergence in the DRC. Understanding the interplay of health, environment, and community response is critical as the nation confronts this public health crisis.
Historical Context of Illnesses in the Congo
The Congo region has a long history of infectious diseases that have significantly impacted the health of its population and shaped public health responses over the years. Diseases such as malaria, yellow fever, and various forms of viral hemorrhagic fevers, including Ebola, have emerged intermittently, raising alarms among health officials and communities alike. The origins of these outbreaks often trace back to ecological changes, human movement, and increased contact between wildlife and humans, particularly in the context of logging, mining, and agricultural expansion.
In the late 1970s, the first recorded cases of Ebola virus in the Congo drew international attention to the region’s vulnerability to viral outbreaks. Subsequent epidemics highlighted both the virulence of the virus and the challenges associated with rapid containment. The lack of robust healthcare infrastructure in many parts of the Democratic Republic of the Congo (DRC) compounded these challenges, leading to delayed responses and heightened mortality rates. Health systems struggled to deal with the complexities of containment and treatment, often exacerbated by socio-political instability and resource limitations.
Moreover, the Congo’s rich biodiversity has acted as a double-edged sword; while it provides valuable resources, it also hosts numerous zoonotic pathogens. These diseases often spill over to human populations, particularly in rural areas where hunting and consumption of bushmeat are commonplace. Inadequate public awareness and education about these risks have contributed to recurring outbreaks, demonstrating the need for improved health education as part of any intervention strategy.
Understanding the historical context of infectious diseases in the Congo is essential to comprehend the current situation and to craft effective responses to recent outbreaks. Each incident adds layers of complexity that influence how health authorities and international organizations respond to emergent threats in this biodiverse but vulnerable region.
Symptoms and Effects of the Congo Illness
The Congo illness, often characterized by a range of debilitating symptoms, poses significant challenges for both those infected and healthcare professionals tasked with diagnosis and treatment. Initial symptoms typically emerge within a short incubation period following exposure, often mimicking other viral infections. For instance, patients commonly experience high fever, severe headaches, muscle pain, and fatigue. As the illness progresses, gastrointestinal symptoms such as nausea and vomiting may occur, alongside abdominal pain and diarrhea. This symptomatology can lead to dehydration, further complicating the clinical picture.
A distinctive feature of the Congo illness is the potential onset of hemorrhagic symptoms, which can include bleeding from mucosal surfaces and, in severe cases, internal bleeding. These manifestations necessitate urgent medical intervention, often resulting in hospitalization for fluid replacement and supportive care. Moreover, the psychological effects of the illness can be profound. Patients may experience significant anxiety related to their symptoms, compounded by the fear of stigmatization associated with infectious diseases. The impact of the disease on mental health should not be overlooked, as the emotional toll can persist even after physical recovery.
When assessing the Congo illness, it is crucial to differentiate it from other known diseases such as Ebola or Lassa fever, which share overlapping clinical features. This can represent a significant challenge for healthcare providers, particularly in regions where multiple infections may circulate simultaneously. Diagnostic tools are vital for accurate identification, requiring both clinical assessment and laboratory testing. Despite the medical advancements available, public health education remains essential to empower communities in recognizing symptoms early, seeking timely treatment, and mitigating the spread of the illness.
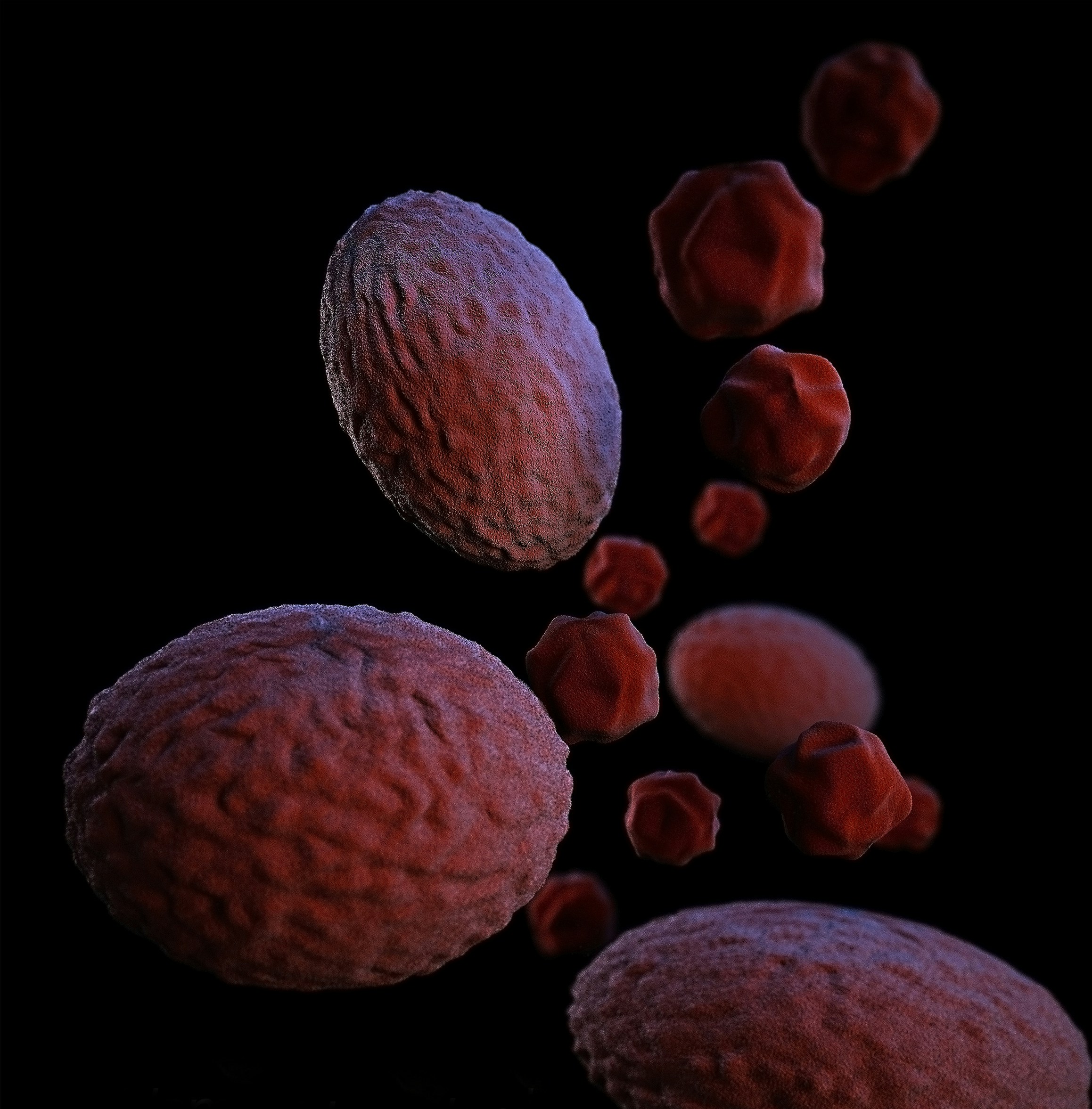
Potential Causes: Exploring Bat and Animal Links
The potential sources of the Congo illness have drawn significant interest from researchers, particularly regarding the role of bats and other wildlife as reservoirs for the pathogens responsible for the outbreaks. Scientific investigation into zoonotic diseases—illnesses that can be transmitted from animals to humans—has clarified the dynamics between wildlife and human health. In various regions, bats are known to harbor numerous viruses, acting as natural reservoirs that can spill over into human populations under certain environmental or ecological conditions.
In the Congo region, specific species of bats have been implicated in the transmission of diseases. Studies indicate that these flying mammals may carry viruses such as the Ebola virus and other filoviruses, which share a pathway for potential transmission to humans. This association raises a pressing question: how do these pathogens jump from their animal reservoirs to human hosts? One leading hypothesis suggests that interactions between humans and bats—whether through deforestation, hunting, or contact with bat droppings—can facilitate this transmission. Such interactions are becoming increasingly common as human populations expand into wildlife habitats.
Moreover, the role of other wildlife species cannot be overlooked. Animals such as rodents and primates also serve as reservoirs for various infectious agents. When these animals come into contact with humans—be it through hunting, consumption, or encroachment upon their natural habitats—they elevate the risk of zoonotic transmission. Researchers continue to explore the complex web of interactions among wildlife, ecosystems, and human activity that contribute to the outbreak of the Congo illness. Understanding these pathways is essential in formulating effective public health strategies and preventive measures to mitigate future outbreaks linked to zoonotic transmission.
Current Research and Investigative Efforts
The recent outbreaks of Congo illness have triggered considerable attention from both local and international health organizations, with significant efforts being dedicated to understanding the disease’s origins, transmission mechanisms, and potential treatments. Research into Congo illness is multifaceted, encompassing epidemiological studies, laboratory investigations, and public health strategies aimed at containment and management.
One of the critical areas of focus for researchers is identifying the reservoirs and vectors associated with the Congo illness. Collaboration between the World Health Organization (WHO) and local health ministries has led to extensive field studies to track the spread of the illness and identify hotspots. These studies are crucial for crafting effective intervention strategies. Current findings suggest that certain ecological conditions may predispose regions to outbreaks, an insight that can inform preventive measures in at-risk areas.
Another significant aspect of ongoing research is the development of diagnostic tools and treatment protocols for Congo illness. Laboratories around the globe are working to identify biomarkers and improve existing diagnostic methods to ensure timely and accurate identification of cases. This is essential, as prompt diagnosis can mitigate the risk of further transmission and enhance patient outcomes.
Investigative efforts also delve into community health education, aiming to raise awareness about the symptoms and transmission routes of Congo illness. By engaging communities through outreach programs, health organizations seek to empower local populations with knowledge that can help reduce stigma and improve the uptake of health services.
In conclusion, current research and investigative efforts are instrumental in combating the Congo illness outbreak. By continuously updating scientific knowledge and disseminating relevant information, researchers and health organizations work towards more effective strategies to manage future outbreaks while safeguarding public health.
Impact on Local Communities and Healthcare Systems
The outbreak of the Congo illness has had profound social and economic implications for affected communities. As the disease spreads, local healthcare systems are increasingly strained. Hospitals and clinics often struggle with a surge in patient numbers, which can overwhelm healthcare personnel who are already contending with limited resources. This situation can lead to longer wait times for treatment, reduced quality of care, and heightened risk of transmission among patients and medical staff alike. Furthermore, the demand for medical supplies and laboratory services exceeds available capacities, compounding challenges faced by healthcare providers.
Communities impacted by the Congo illness are also experiencing economic disruption. Many individuals rely on daily wages, which can be severely affected if they are forced to quarantine or if local businesses close to mitigate the virus’s spread. The decrease in workforce availability impacts productivity, leading to a deterioration of economic stability within these regions. Families may find themselves in precarious financial situations, often exacerbating preexisting vulnerabilities linked to poverty and limited access to basic necessities.
In the face of these challenges, local organizations are stepping up to provide assistance and support. They play a critical role in educating communities about the Congo illness, promoting public health practices, and offering emotional and material support to those affected. Initiatives may include setting up temporary health facilities, deploying trained healthcare workers, and distributing essential supplies such as food and hygiene kits. Collaborative efforts among local organizations, governmental entities, and international aid agencies are vital in managing the outbreak, fostering resilience, and ensuring a coordinated response to safeguard community health.
Overall, the Congo illness poses significant challenges for affected communities, amplifying the need for a robust response that addresses both healthcare and economic impacts.
Preventive Measures and Health Education
The recent outbreaks of Congo illness necessitate a robust response strategy aimed at curbing the transmission and impact of the disease. To achieve this, health authorities have devised a multi-faceted approach that includes health education campaigns, community engagement initiatives, and, where applicable, vaccination efforts. These strategies play a crucial role in raising awareness and promoting essential health practices within affected communities.
Health education campaigns are fundamental in disseminating vital information about the Congo illness, its symptoms, and the means of transmission. By utilizing various platforms, including local media, community meetings, and informational pamphlets, health officials can effectively reach a wider audience. These campaigns provide residents with actionable steps to protect themselves and their families, such as practicing good hygiene, avoiding contact with wild animals, and seeking medical attention promptly if symptoms appear.
Vaccination efforts have also been a cornerstone in the fight against Congo illness, particularly in areas with a high incidence of the disease. Vaccines can drastically reduce the risk of infection, and health organizations are mobilizing to provide accessible immunization services. In tandem with vaccination, community engagement initiatives strive to involve local leaders and organizations to ensure that prevention messages resonate culturally and contextually with the population. Such collaborations foster trust and encourage communal support for health initiatives.
Moreover, facilitating open discussions surrounding health issues enables communities to share concerns and solutions, thereby enhancing adherence to preventive measures. By actively involving community members in the planning and implementation of preventive efforts, the sustainability of health education campaigns improves significantly. Overall, these preventive measures and health education initiatives are vital for diminishing the spread of Congo illness and ensuring the well-being of affected populations.
International Response and Collaboration
The emergence of the Congo illness has prompted a significant response from international health organizations, governments, and non-governmental organizations (NGOs). Following the recent outbreaks, various stakeholders recognized the urgent need for coordinated action to mitigate the effects of this disease on vulnerable populations. Key players such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have mobilized resources and expertise to provide technical assistance and support to affected regions.
Partnerships are essential in effectively addressing the complexities associated with the Congo illness. Collaborative efforts often involve a multi-faceted approach, which includes the sharing of data, research findings, and best practices. For instance, international collaborations have enabled researchers to better understand the transmission dynamics of the disease, ultimately informing prevention strategies and treatment protocols. Additionally, partnerships between local health authorities and international agencies enhance the delivery of medical supplies and other critical resources.
Funding plays a pivotal role in sustaining these initiatives. Numerous governments and international bodies have allocated financial resources aimed at bolstering healthcare systems in regions heavily affected by the Congo illness. This funding is typically directed towards enhancing outbreak surveillance, improving diagnostic capabilities, and facilitating health education campaigns aimed at raising awareness about prevention measures. NGOs also contribute to this funding landscape by launching targeted projects, which often focus on community engagement and the promotion of health-seeking behaviors.
In summary, the international response to the Congo illness underscores the importance of collaboration across multiple sectors. Coordinated efforts ensure a more comprehensive approach to outbreak control, reflecting a commitment to protecting public health and fostering resilience in communities that bear the brunt of these outbreaks. As the situation evolves, ongoing engagement and partnership will be vital to effectively safeguard those at risk and to unravel the complex factors underlying the disease’s emergence.
Future Outlook: What Lies Ahead for the Congo Illness
The recent outbreaks of Congo illness have raised significant concerns regarding public health preparedness and response strategies. Looking ahead, it is increasingly evident that ongoing research will play a crucial role in understanding the epidemiology of this disease, its transmission patterns, and effective treatment protocols. Predictions based on current data suggest that with advancements in technology and collaborative efforts among global health organizations, the prevention and management of Congo illness can markedly improve.
One of the primary factors influencing the future trajectory of Congo illness is the emphasis on heightened global awareness of emerging infectious diseases. Increased surveillance and reporting will be essential as outbreaks may occur sporadically, often in under-resourced areas. This necessitates a multi-faceted approach that leverages data sharing, enhanced diagnostic capabilities, and training of healthcare professionals to identify and manage potential cases early.
Preparedness is key in combating similar health crises. Countries with demonstrated vulnerabilities must prioritize the development of robust healthcare infrastructure while also implementing effective public health policies. Vaccine research and development will take center stage; as vaccine candidates progress through trials, their efficacy and accessibility may define future outbreak management strategies. Collaborative platforms involving governments, non-governmental organizations, and academic institutions are vital for fostering innovation in vaccine and therapeutic developments.
Furthermore, public education campaigns about the risk factors associated with Congo illness are critical in evolving community response mechanisms. Educating populations on the importance of hygiene practices and knowing the symptoms can significantly reduce the spread of infection. Overall, the future of Congo illness relies heavily on global solidarity and proactive measures to address potential outbreaks, ensuring that, as a global community, we are prepared to face the challenges posed by emerging infectious diseases.