Introduction to HMPV Virus
Human Metapneumovirus (HMPV) is a notable member of the Metapneumovirus genus, which was first identified in the Netherlands in 2001. This RNA virus is recognized as a significant respiratory pathogen that affects individuals of all ages but is particularly concerning for infants, the elderly, and immunocompromised patients. HMPV is now viewed as a noteworthy cause of respiratory illnesses, including bronchiolitis and pneumonia, often leading to hospitalization during the colder months when respiratory viruses are prevalent.
The virus spreads primarily through respiratory droplets when an infected individual coughs or sneezes. It can also be transmitted by direct contact with contaminated surfaces. This mode of transmission accentuates the challenges faced in preventing outbreaks, especially in communal settings, such as schools and healthcare facilities. As a relatively recent discovery in the field of virology, HMPV has drawn significant attention due to its similarities with other well-known respiratory viruses, such as respiratory syncytial virus (RSV) and human parainfluenza viruses.
The characteristics of HMPV — including its genetic variability and its capacity for evading the host immune response — complicate diagnostic approaches and treatment protocols. Despite its increasing recognition, many clinicians remain unaware of HMPV’s potential impact on public health. Consequently, ongoing research into the virus’s transmission, clinical manifestations, and long-term effects is crucial. This further establishes the importance of awareness regarding HMPV, both for healthcare professionals and the general population. By enhancing understanding of this respiratory pathogen, we can aim for improved management, prevention, and ultimately better health outcomes for affected individuals.
Current Trends in HMPV Cases
The Human Metapneumovirus (HMPV) has emerged as a significant concern within global public health, with recent data indicating an uptick in reported cases across various regions. According to the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), surveillance data reveals that HMPV cases have seen a notable increase, particularly during the spring months of the year. This seasonal trend aligns with respiratory virus patterns, suggesting that HMPV may behave similarly to other respiratory viruses such as RSV and influenza.
Geographically, the highest incidence rates of HMPV infections have been documented in North America and Europe, though cases have been reported globally, including in Asian and African nations. Recent statistics indicate that certain demographics, particularly young children and the elderly, are disproportionately affected. Hospitalization rates due to respiratory illnesses caused by HMPV have risen, stressing healthcare systems in regions where the virus is endemic.
Health organizations have emphasized the importance of ongoing monitoring and reporting as these trends unfold. Pediatric populations have shown a significant vulnerability, with a rise in severe cases leading to increased pediatric hospital admissions. Adult cases, although fewer, also display considerable morbidity, especially among older adults with preexisting health conditions.
Furthermore, a lack of vaccination options and antiviral therapies specifically targeting HMPV adds to the urgency of understanding these trends. Researchers are calling for further studies that could unravel the underlying causes of this surge in cases, which may be influenced by factors such as climate change and population density. Maintaining public health communication and awareness becomes imperative as we navigate the challenges posed by this mystery virus.
Symptoms and Transmission of HMPV
Human Metapneumovirus (HMPV) is an emerging viral pathogen that primarily affects the respiratory system. Understanding the symptoms associated with HMPV is critical for early identification and management. The disease often presents similarly to other viral respiratory infections, making differentiation somewhat challenging. Common symptoms include a persistent cough, nasal congestion, fever, wheezing, and shortness of breath. Patients may also experience fatigue and a sore throat. In some cases, particularly among younger children, older adults, or those with compromised immune systems, the infection can escalate to severe respiratory illness, requiring medical intervention.
The transmission of HMPV occurs predominantly through respiratory droplets released when an infected person coughs or sneezes. Close contact with an infected individual can facilitate the spread of the virus, particularly in communal settings such as schools, daycare facilities, and nursing homes. Surface contamination is another crucial aspect of HMPV transmission; the virus can survive on surfaces for several hours. Therefore, touching contaminated surfaces followed by contact with the face can also lead to infection. Factors that contribute to its transmission include crowded environments, inadequate ventilation, and seasonal trends, as HMPV commonly circulates during the late winter and early spring months.
Increased awareness of the symptoms and modes of transmission of HMPV is pivotal for controlling outbreaks. As the virus can be mistaken for other respiratory illnesses, individuals should be vigilant about the range of symptoms and their potential exposure to infected persons. By promoting good hygiene practices, such as regular hand washing and the use of masks in high-risk settings, the spread of HMPV can be minimized, ultimately contributing to public health safety.
HMPV’s Impact on Vulnerable Populations
The human metapneumovirus (HMPV) presents significant health risks, particularly for vulnerable populations such as children, the elderly, and individuals with compromised immune systems. Emerging research indicates that these groups experience higher rates of morbidity and mortality associated with HMPV infections, leading to detrimental health outcomes that necessitate urgent attention and targeted healthcare strategies.
For young children, especially infants, HMPV can lead to acute respiratory infections prompting visits to healthcare facilities. The virus often manifests with symptoms similar to other viral upper respiratory infections, including cough, fever, and wheezing. These symptoms can escalate in infants and toddlers, resulting in bronchiolitis or pneumonia, thereby requiring hospitalization in severe cases. Caregivers must be vigilant for early indicators of severe illness, particularly during peak seasons when HMPV circulates more frequently.
Similarly, the elderly face increased risks. Older adults often exhibit weakened immune systems, making them more susceptible to respiratory viruses like HMPV. The complications stemming from an HMPV infection in this demographic can be grave, potentially leading to exacerbations of chronic diseases such as chronic obstructive pulmonary disease (COPD) or heart failure. Effective management of secondary infections, coupled with monitoring for respiratory distress, is critical during an HMPV outbreak.
Individuals with compromised immune systems, including those undergoing cancer treatment or with autoimmune disorders, constitute another high-risk group. Their bodies may struggle to mount an adequate immune response against the HMPV, leading to prolonged illness and complications such as bacterial superinfections. Thus, it is essential that healthcare providers adopt a proactive approach to screening and prevention strategies for these at-risk populations.
Ultimately, understanding the nuances of HMPV’s impact on these vulnerable individuals underscores the importance of tailored healthcare interventions aimed at minimizing risks and improving outcomes among those affected.
Preventative Measures Against HMPV
As global health organizations grapple with the rising cases of Human MetaPredominant Virus (HMPV), it becomes increasingly vital for individuals and communities to adopt effective preventative measures aimed at reducing the risk of HMPV transmission. These measures largely revolve around personal hygiene practices, potential vaccination developments, and adherence to public health recommendations.
Maintaining good hygiene practices serves as a cornerstone in combating HMPV spread. Regular hand washing with soap and water, particularly after being in public spaces, helps eliminate viruses from the hands and reduces the likelihood of transmission. When soap and water are not readily available, the use of hand sanitizer containing at least 60% alcohol is advisable. Additionally, avoiding close contact with infected individuals and refraining from touching one’s face, particularly the eyes, nose, and mouth, can further minimize risk.
Current research into HMPV has led to discussions regarding the possibility of developing a vaccination. While no vaccine is currently available, staying informed on advancements in vaccine development is crucial for community health. Vaccination has historically demonstrated efficacy in reducing the spread of viruses; thus, public health initiatives should include timely updates regarding potential HMPV vaccines.
Public health officials recommend several preventive measures, including the practice of respiratory etiquette. This involves covering coughs and sneezes with a tissue or elbow to prevent respiratory droplets from dispersing in the environment. Furthermore, limiting gatherings during peak transmission seasons may also help reduce the overall incidence of HMPV. In addition, educating communities about the significance of reporting symptoms and seeking medical advice when necessary can bolster collective efforts in managing and mitigating outbreaks.
In conclusion, understanding and implementing these preventive measures can significantly contribute to reducing the transmission of HMPV, thereby safeguarding personal health and the well-being of communities. By fostering a proactive approach to hygiene, remaining apprised of vaccination potential, and adhering to public health guidelines, individuals can play a pivotal role in curbing the spread of this mystery virus.
Diagnosis and Treatment of HMPV Infections
The diagnosis of human metapneumovirus (HMPV) infections is primarily conducted through a combination of clinical evaluations and laboratory tests. Clinicians begin by assessing the patient’s medical history and symptoms, which often resemble those of other respiratory viral infections. Common symptoms include fever, cough, wheezing, and difficulty breathing, which are typically evaluated during a physical examination. Given the overlapping nature of presentations among various respiratory viruses, accurate diagnosis may necessitate specific laboratory testing.
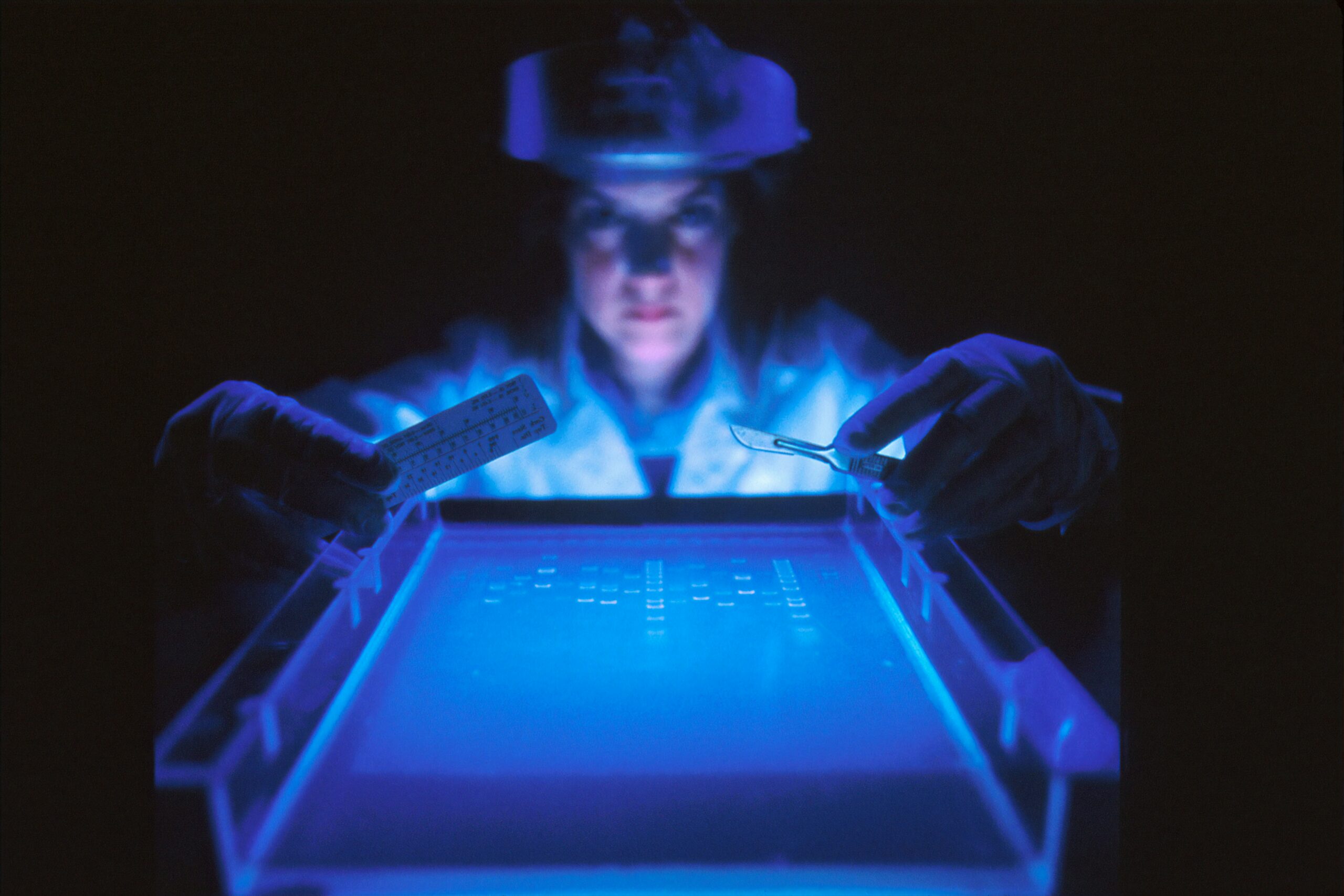
Laboratory tests for HMPV include molecular assays such as polymerase chain reaction (PCR), which can detect the viral RNA in respiratory samples. This method is considered the gold standard due to its high sensitivity and specificity. Additionally, antigen detection tests may be employed for rapid diagnosis, although they vary in reliability. Serological tests assessing antibodies against HMPV can also be informative, particularly in cases when acute infection is suspected, yet these are less commonly used in clinical settings for immediate diagnosis.
Regarding treatment, there are no specific antiviral medications approved exclusively for HMPV. Management typically focuses on alleviating symptoms and supporting the respiratory system. Patients with mild symptoms may be treated with supportive care, including rest, hydration, and over-the-counter medications to relieve fever and discomfort. For those with more severe respiratory issues, hospitalization may be necessary. Treatments can involve supplemental oxygen, bronchodilators, and corticosteroids to reduce inflammation in the airways.
In certain instances, particularly in high-risk populations such as young children or immunocompromised individuals, experimental therapies or monoclonal antibodies may be considered. However, the overall management of HMPV remains largely symptomatic, underscoring the need for further research to develop targeted antiviral therapies.
Comparison with Other Respiratory Viruses
The Human Metapneumovirus (HMPV) is one of several viruses that can cause respiratory infections, alongside more widely recognized pathogens such as influenza and Respiratory Syncytial Virus (RSV). Understanding the similarities and differences among these viruses can provide valuable context for public health initiatives and individual awareness.
HMPV typically presents with symptoms similar to those of influenza and RSV, including cough, fever, and wheezing. However, the severity of symptoms can vary significantly among these viruses. Influenza is known for its sudden onset and high fever, while RSV often leads to bronchiolitis in infants and can cause severe respiratory distress. In contrast, HMPV’s clinical presentation may range from mild upper respiratory symptoms to severe lower respiratory tract disease in vulnerable populations, such as young children and the elderly. This variability in symptomatology can complicate diagnosis and treatment.
In terms of transmission, HMPV, like its counterparts, spreads through respiratory droplets when an infected person coughs or sneezes. Additionally, it can survive on surfaces, thereby facilitating indirect transmission. Although HMPV shares these transmission characteristics with influenza and RSV, the general public may have a greater awareness of the seasonal spikes associated with influenza outbreaks, leading to more considerable public health responses in its case. Notably, the public health response to HMPV is often less robust than that for influenza and RSV, primarily due to a lack of widespread recognition and understanding of HMPV.
In conclusion, comparing HMPV to influenza and RSV illuminates its position within the broader spectrum of respiratory viruses. Despite notable overlaps in symptoms and modes of transmission, the distinct public health approaches reflect varying levels of awareness and understanding regarding HMPV’s impact on respiratory health.
Research and Future Directions
The ongoing research surrounding Human Metapneumovirus (HMPV) has become increasingly vital as cases continue to rise. Scientists are actively investigating various aspects of this virus, with a strong emphasis on vaccine development. Numerous studies have been initiated to evaluate potential vaccine candidates that could provide immunity against HMPV. These vaccines aim not only to mitigate the effects of the virus in infected individuals but also to prevent its spread among populations, particularly vulnerable groups such as young children and the elderly.
In addition to vaccine research, epidemic modeling has gained significant traction in understanding the patterns and dynamics of HMPV transmission. Researchers are employing advanced computational models to simulate various scenarios regarding the outbreak of this virus. These models can assist public health officials in strategizing effective interventions, determining potential hotspots, and planning resource allocation for healthcare facilities. By integrating real-world data with theoretical frameworks, scientists hope to predict future trends in HMPV cases and inform preparedness plans accordingly.
Another area of focus is the study of immune responses to HMPV. Understanding how the immune system reacts to this particular virus is crucial for developing effective treatment strategies and vaccines. Researchers are exploring the types of antibodies produced during infection and how these may confer protection against future infections. Insights gained from these studies could pave the way for enhancing vaccine efficacy and informing therapeutic options tailored to counteract HMPV’s impacts.
Overall, the future implications of research into HMPV are promising. By advancing knowledge in vaccine development, epidemic modeling, and immune responses, researchers are not only addressing the immediate challenges posed by HMPV but also contributing to a stronger public health framework. This multifaceted approach will ultimately foster improved disease management and preparedness for future outbreaks of HMPV and other respiratory viruses.
Conclusion and Call to Action
In recent years, the emergence of HMPV (Human Metapneumovirus) has brought a renewed focus on respiratory illnesses that can significantly impact public health. Throughout this blog post, we have explored the nature of HMPV, its symptoms, transmission methods, and the demographics most affected. This relatively understudied virus has been linked to respiratory infections globally, emphasizing the necessity for heightened awareness and research. As cases rise, the medical community and general public must recognize the importance of preventive measures and collective action.
HMPV is characterized by a range of respiratory symptoms, often resembling those caused by other common viruses such as influenza or RSV (Respiratory Syncytial Virus). Its ability to spread through respiratory droplets reinforces the importance of practicing good hygiene, such as frequent handwashing and wearing masks in crowded settings. Understanding HMPV and its implications can empower individuals and communities to take proactive steps in safeguarding their health. Public health campaigns play a crucial role in educating the populace about symptoms and when to seek medical attention.
Moreover, collaboration among health authorities, researchers, and community members is essential to combat the threat posed by infectious diseases like HMPV. Staying informed about updates and advancements in treatment and prevention can further enable individuals to contribute positively to their communities. We encourage readers to engage with local health initiatives, whether through volunteering, sharing information, or participating in awareness campaigns. By fostering a culture of vigilance and readiness, we can better protect ourselves and those around us from the lingering threats of respiratory viruses.
As cases of HMPV and similar viruses continue to be monitored, our collective awareness and action can make a substantial difference in managing public health responses and outcomes. Let us commit to being informed and involved in the fight against respiratory illnesses, together.


I have observed that costs for internet degree authorities tend to be a fantastic value.